Vascular rejection has been traditionally considered a severe form of acute rejection characterized by infiltration of mononuclear cells beneath the endothelium or by the presence of arteritis. Though initially reported as an aggressive form of T-cell mediated rejection with poor response to T-cell targeted therapy, newer findings suggest a strong association with alloantibodies.
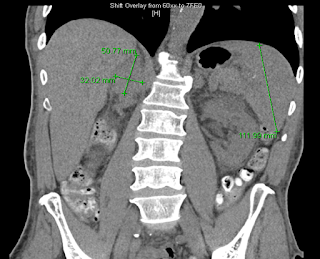
Study from France analyzed 302 patients with biopsy-proven rejection and identified 4 subtypes of acute rejection with different outcomes (Figure): T-cell-mediated vascular rejection (9%), antibody-mediated vascular rejection (21%), T-cell-mediated rejection without vasculitis (46%), and antibody-mediated rejection without vasculitis (24%).
Antibody-mediated vascular rejection manifested a median of 1.1 months (0.4–4.4) post-transplant and had the worst prognosis of the four subtypes. Moreover, 71% of cases of vascular rejection, which were mostly graded as v1 and v2 arteritis by the Banff schema, were associated with donor-specific antibodies (DSA).
Therefore, it seems that the majority of cases of vascular rejection are associated with DSA and therapies to remove and decrease alloantibody production may be warranted. Indeed, this study suggested that antibody-directed treatment involving plasmapheresis, IVIG and rituximab led to better outcomes in this subpopulation. As of today, v1 and v2 vascular lesions are not accounted by the Banff classification in the antibody-mediated rejection category.
Alloantibodies may bind to endothelium antigens and activate complement, attracting mononuclear cells which express Fc and adherence receptors, initiating the process of vascular infiltration.
How will this affect our practice? Whenever a biopsy shows a component of vascular rejection, one must send the serum for alloantibody testing, even if biopsy is not classic for antibody-mediated rejection. Furthermore, antibody-directed treatment strategies should be considered, in particular if no response to initial therapy and evidence of DSA. The ideal treatment of the different severities of vascular rejection still remain to be determined.