
Congenital nephrotic syndrome only makes up between 2-8% of all forms of nephrotic syndrome, but is a hot topic in that there are numerous genes continuously being identified which are helping to advance our understanding of podocyte biology.
A list of nephrotic syndrome-causing genes identified thus far with a brief description of each is listed below:
1. nephrin (NPHS1): this was the first gene identified which causes congenital nephrotic syndrome of the Finnish type. As shown in the cartoon above, nephrin is a major component of the slit diaphragm.
2. podocin (NPHS2): this was the next gene identified and is the most commonly mutated gene causing steroid-resistant nephrotic syndrome.
3. WT1: this is the Wilms Tumor gene which acts as a transcriptional activator or repressor and is essential for proper development of the genitourinary system.
4. LAMB2: this is a gene for laminin, one of the components of the glomerular basement membrane.
5. PLCE1: this surprising gene--which unlike the others does not play an important structural role in the slit diaphragm--encodes an isoform of phospholipase epsilon gene. Individuals with this mutation actually show an increased responsiveness towards steroid therapy.
6. alpha-actinin-4: this gene encodes an actin filament-crosslinking protein which can cause congenital FSGS.
7. TRPC6: this gene encodes a calcium channel expressed in podocytes, and mutations in it can result in congenital FSGS.
This list of genes causing congenital nephrotic syndrome is likely to expand as there are families with this condition which do not link to any of the above loci.
 Polyarteritis nodosa (PAN) and Microscopic polyangiitis (MPA) are two vasculitides which were previously grouped together.
Polyarteritis nodosa (PAN) and Microscopic polyangiitis (MPA) are two vasculitides which were previously grouped together. 

 The M3 subtype of acute myelogenous leukemia--also known as acute promyelocytic leukemia--is one of the most responsive forms of leukemia, as the addition of all-trans retinoic acid (ATRA) is known to overcome the maturation block in affected lymphocytes.
The M3 subtype of acute myelogenous leukemia--also known as acute promyelocytic leukemia--is one of the most responsive forms of leukemia, as the addition of all-trans retinoic acid (ATRA) is known to overcome the maturation block in affected lymphocytes. 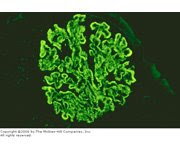









 The reason for the increased use of catheters likely stems from the fact that there is an increasing rate of primary fistula failure--typically caused by failure to mature or thrombosis, possibly related to a sicker, more vasculopathic, aging population--and the decreased use of AV grafts. A recent KDOQI workgroup in 2006 re-emphasized that the goal of the Fistula First campaign should be a functional AV fistula, not simply the insertion of an AV fistula with a poor chance at maturing. As one vasscular surgeon at our hospital points out, the initiative should be "Patient First" rather than simply "Fistula First." In other words, the vascular access strategy should be individualized to the patient--meaning that for elderly, vasculopaths with poor native vessels who are anticipated to require dialysis in the near future, it may be appropriate to begin with a AV graft rather than attempting an AV fistula with little chance of success.
The reason for the increased use of catheters likely stems from the fact that there is an increasing rate of primary fistula failure--typically caused by failure to mature or thrombosis, possibly related to a sicker, more vasculopathic, aging population--and the decreased use of AV grafts. A recent KDOQI workgroup in 2006 re-emphasized that the goal of the Fistula First campaign should be a functional AV fistula, not simply the insertion of an AV fistula with a poor chance at maturing. As one vasscular surgeon at our hospital points out, the initiative should be "Patient First" rather than simply "Fistula First." In other words, the vascular access strategy should be individualized to the patient--meaning that for elderly, vasculopaths with poor native vessels who are anticipated to require dialysis in the near future, it may be appropriate to begin with a AV graft rather than attempting an AV fistula with little chance of success.








 Heavy metals & the kidney are an interesting topic all-around. Aberrant metabolism of heavy metals such as iron, copper, lead all contribute to significant renal pathology. And you can add the heavy metal
Heavy metals & the kidney are an interesting topic all-around. Aberrant metabolism of heavy metals such as iron, copper, lead all contribute to significant renal pathology. And you can add the heavy metal 



















